Keywords: lower limb rehabilitation; postoperative rehabilitation; NASA Anti Gravity Treadmill
Abstract:
To investigate the effects of body weight support (BWS) and walking speed on cardiovascular responses during walking on an antigravity treadmill early after unilateral and bilateral total knee arthroplasty (TKA).
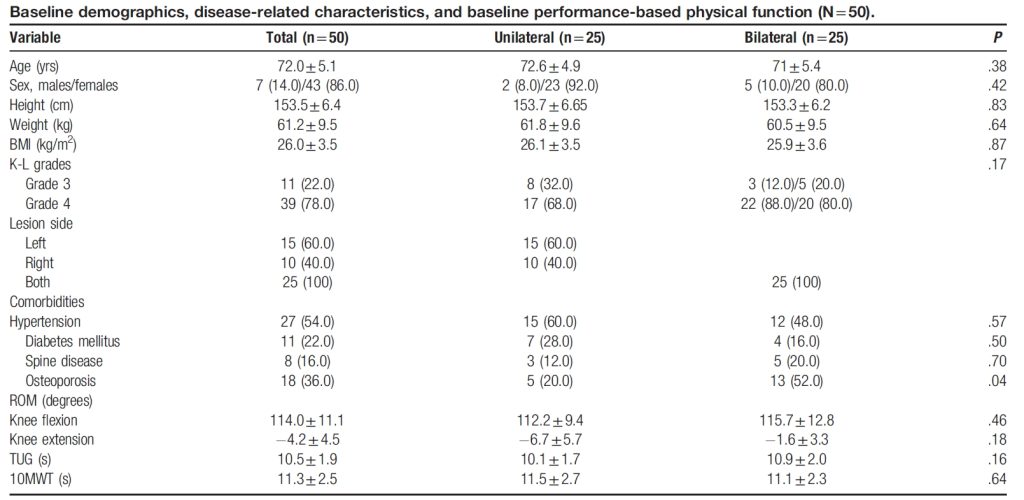
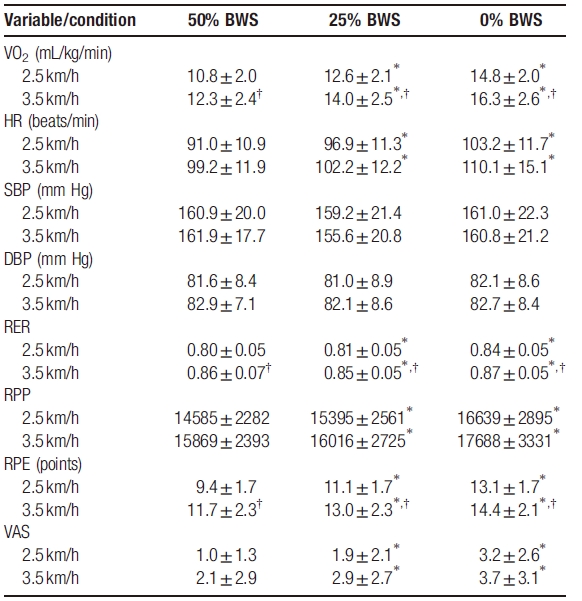
This study was cross-sectional in design. Fifty patients (7 males and 43 females; mean age 72.0±5.1 years) participated in this study 4 weeks after unilateral (n=25) and bilateral (n=25) primary TKA. Subjects walked on an antigravity treadmill at speeds of 2.5 km/h and 3.5 km/h with 3 levels of BWS (50%, 25%, and 0%). Cardiovascular responses were monitored by measuring oxygen consumption (VO2), heart rate (HR), systolic and diastolic blood pressure (SBP/DBP), respiratory exchange ratio (RER), and rate-pressure product (RPP). The Borg rate of perceived exertion (RPE) score and the visual analogue scale (VAS) for knee pain were recorded immediately after each trial.
There were no significant differences in cardiovascular response between the unilateral and bilateral TKA groups. In repeated measures ANOVA, VO2 levels, HR, RPP, RPE, RER, and VAS were significantly increased in proportion to 3 BWS levels (50%, 25%, and 0%) in the unilateral and bilateral TKA groups, respectively. Meanwhile, SBP and DBP are not affected by BWS differences. At a speed of 3.5 km/h, the VO2, RPE and RER values were higher than those at 2.5 km/h under the same BWS conditions.
The article is cited in:
Observational Study
The test was performed on an anti-gravity treadmill (Fremont, CA). Heart rate was monitored using a waterproof chest strap transmitter (Polar T34, Polar Electro, Inc, Kempele, Finland). Before stepping on the treadmill, the subjects put on specially made shorts that were worn to the level of the subject’s anterior superior iliac spine (ASIS). After putting on the shorts, the subject stepped into the opening of the treadmill. The metal frame holding the balloon was raised to the level of the subject’s ASIS. The shorts with zipper lining were then attached to the balloon to create an airtight seal. Before the test, the physical therapist adjusted the air pressure in the chamber to apply the appropriate lift to each subject. The first phase began with the subject correctly positioned in the . The subject began walking at a speed of 2.5 km/h with 50% of body weight. The body weight was adjusted after each trial so that the subject was tested at 50%, 25%, and 0% of body weight. The test was then repeated at a speed of 3.5 km/h under the same body weight conditions. Each trial lasted 2 min, with at least 1 min between trials.
Testing was terminated at the patient’s request or if gait instability (defined as marked instability and inconsistency from first to next step) developed or cardiovascular decompensation became evident (assessed according to the American College of Sports Medicine guidelines)。
Results showed that BWS had a greater impact on cardiovascular responses and knee pain than walking speed, although it is important to note that the difference in the latter was only 1 km/h. When we performed a multiple linear regression analysis defining VO2 as a function of walking speed and BWS for each set of conditions, the following equation emerged: VO2= 1.5 v+0.1 BWS+3.1. That is, VO2 can be derived from various combinations of BWS and walking speed, with 15% BWS and a speed of 1 km/h having similar VO2 values. These results have important clinical implications because they provide clues as to how to adjust BWS and walking speed conditions on an antigravity treadmill in the early postoperative period to provide exercise of appropriate intensity without exacerbating knee pain. The intensity of cardiorespiratory exercise can be measured by assessing RPE. Controlling for BWS and gait speed, results on the RPE scale ranged from 10 to 14 points; meaning patients rated the test as “fairly light” to “somewhat difficult.” Moderate-intensity aerobic exercise typically results in an RPE score of 12 to 14; therefore, the exercise intensities used in this study appear to be appropriate. Furthermore, gait speed had no significant main effect on VAS, whereas BWS had a significant main effect on VAS. Taking these findings into account, when conducting gait training on an antigravity treadmill in the early postoperative period, it is best to first increase the gait speed from 2.5 km/h to 3.5 km/h at the maximum BWS level (50% BWS) and then based on The degree of knee pain gradually decreased after BWS surgery. Here, we set the pace as 2.5 km/h and 3.5 km/h because 2.5 km/h is the average self-selected pace for community-dwelling elderly people suggested by Singh et al., while 3.5 km/h is closest to what our study suggested. Average walking speed measured during 10MWT (0.9 m/s). Gait speed is a key factor in diagnosing sarcopenia and has the potential to predict future functional decline and fall risk. Additionally, decreased gait speed is associated with multiple health-related factors, including disability, hospitalization, loss of independence, and mortality. Therefore, providing BWS in the early postoperative period allows patients to perform appropriate levels of aerobic exercise at a faster pace. While walking aids such as crutches, walkers, and canes can support body weight, their effectiveness is limited because patients are unable to maintain a high enough walking speed for an appropriate period of time during exercise, and use of walking aids can significantly alter joints and gait mechanics.
Finally, we found that cardiovascular responses in the unilateral TKA group were similar to those in the bilateral TKA group; the only difference was the significance of some values after post hoc analysis. There were no significant differences between the two groups on performance-based physical functioning.
Conclusion:
This study has several limitations. First, the number of patients in each group was small. Second, we used 50%, 25%, and 0% BWS; however, a previous study examining unloading on an antigravity treadmill showed that the device was most accurate in the 10% to 30% BWS range; the differences were relatively large in the higher (0% BWS) and lower (70%-80% BWS) ranges. Of note, in the “0% BWS” condition, the antigravity treadmill actually provided approximately 7% BWS. These limitations should be considered when interpreting cardiovascular responses, especially those recorded at 0% BWS. In addition, these limitations should also be considered when using other BWS systems. Third, the same sequence of BWS was used for each participant; this may have affected their pain scores. Finally, our patients received inpatient physical therapy 4 weeks before testing, and this extensive rehabilitation may have affected cardiovascular responses. Therefore, these findings cannot be generalized to patients who did not receive rehabilitation at the same postoperative time point.